![]()
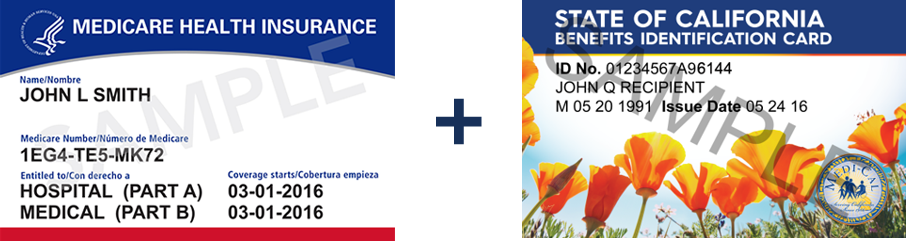
Medi-Cal Managed Care Enrollment—Provider Fact Sheet
Crossover Billing Provider Toolkit
Starting January 2023, most dually eligible beneficiaries who were not already enrolled in Medi-Cal managed care were enrolled in Medi-Cal plans in 2023. Medi-Cal plans provide wraparound services and care coordination dual eligible beneficiaries, particularly for Long-Term Services and Supports.
DHCS sent beneficiary notices by November 1 and December 1, 2022. For more information on Medi-Cal managed care plan choices, please visit Health Care Options.
Joining a Medi-Cal Managed Care Plan will NOT Change Your Medicare Benefits
Your Medicare benefits will not change after you join a Medi-Cal plan. Joining a Medi-Cal plan will not affect your Medicare providers or choice of Medicare Advantage plan or Original Medicare. Medicare providers do not need to be in the Medi-Cal plan network to continue to provide you care. You can still see your Medicare providers and go to the hospital where you see your Medicare doctors.
- Prior to January 1, 2023, over 70 percent (over 1.1 million) of beneficiaries dually eligible for Medicare and Medi-Cal were enrolled in Medi-Cal managed care plans.
- Starting January 2023, Medi-Cal health coverage for most remaining dually eligible beneficiaries changed from Fee-For-Service (FFS) Medi-Cal to Medi-Cal Managed Care.
- Medi-Cal managed care enrollment does NOT affect a beneficiary’s Medicare providers or Medicare Advantage plan.
- Medicare providers do NOT need to be in the Medi-Cal managed care network to continue to provide care to their Medicare beneficiaries.
- Medi-Cal plans provide many benefits, including those that “wrap around” Medicare. As part of CalAIM, Medi-Cal plans statewide are expanding the type of services that could benefit dual eligible beneficiaries, including Enhanced Care Management and Community Supports. These services are not available through Medi-Cal fee-for-service.
Medi-Cal Beneficiary Notices and Outreach Materials
DHCS sent out notices explaining the key elements of this transition on November 1, 2022 Those notices and video presentations explaining the transition are available on the Medi-Cal Managed Care Enrollment Outreach Webpage.
Information by County
Counties where dually eligible beneficiaries are enrolled in Medi-Cal managed care in 2023: Alameda, Alpine, Amador, Butte, Calaveras, Colusa, Contra Costa, El Dorado, Fresno, Glenn, Imperial, Inyo, Kern, Kings, Madera, Mariposa, Mono, Nevada, Placer, Plumas, Sacramento, San Benito, San Francisco, San Joaquin, Sierra, Stanislaus, Sutter, Tehama, Tuolumne, Tulare, and Yuba counties.
Counties where dually eligible beneficiaries were already enrolled in Medi-Cal managed care prior to 2023: Del Norte, Humboldt, Lake, Lassen, Los Angeles, Marin, Mendocino, Merced, Modoc, Monterey, Napa, Orange, Riverside, San Bernardino, San Diego, San Luis Obispo, San Mateo, Santa Barbara, Santa Clara, Santa Cruz, Shasta, Siskiyou, Solano, Sonoma, Trinity, Ventura, and Yolo counties.
Medi-Cal Matching Plan Policy: In 12 large/medium counties, beneficiaries who were already enrolled in a Medicare Advantage plan were enrolled in the “matching” Medi-Cal plan, under the same parent organization, if matching plan was available. These beneficiaries will receive the 2B notices mentioned above under Medi-Cal Beneficiary Notices.
Beneficiaries who were not enrolled in a Medicare Advantage plan, or in a Medicare Advantage plan without a matching Medi-Cal plan, could choose a Medi-Cal plan using materials they received in fall 2022. These beneficiaries will receive the 2A notices mentioned above under Medi-Cal Beneficiary Notices.
Additional Resources
- Visit Health Care Options for more information on the Medi-Cal plan choices in your county
- For free counseling on Medicare options, contact the Health Insurance Counseling and Advocacy Program (HICAP)
- Call the Medicare Medi-Cal Ombudsman if you need help with a problem that your health plan has not been able to resolve
- For more information on the Medi-Cal managed care transition, please visit this webpage at the California Department of Health Care Services: Statewide Medi-Cal Managed Care Enrollment for Dual Eligible Beneficiaries.
