The California Department of Health Care Services (DHCS) is committed to achieving excellence in the quality and equity of care for Medi-Cal members. Through broader efforts focused on
Medi-Cal Transformation, as well as through the ambitious
2022 Comprehensive Quality Strategy, DHCS outlined a
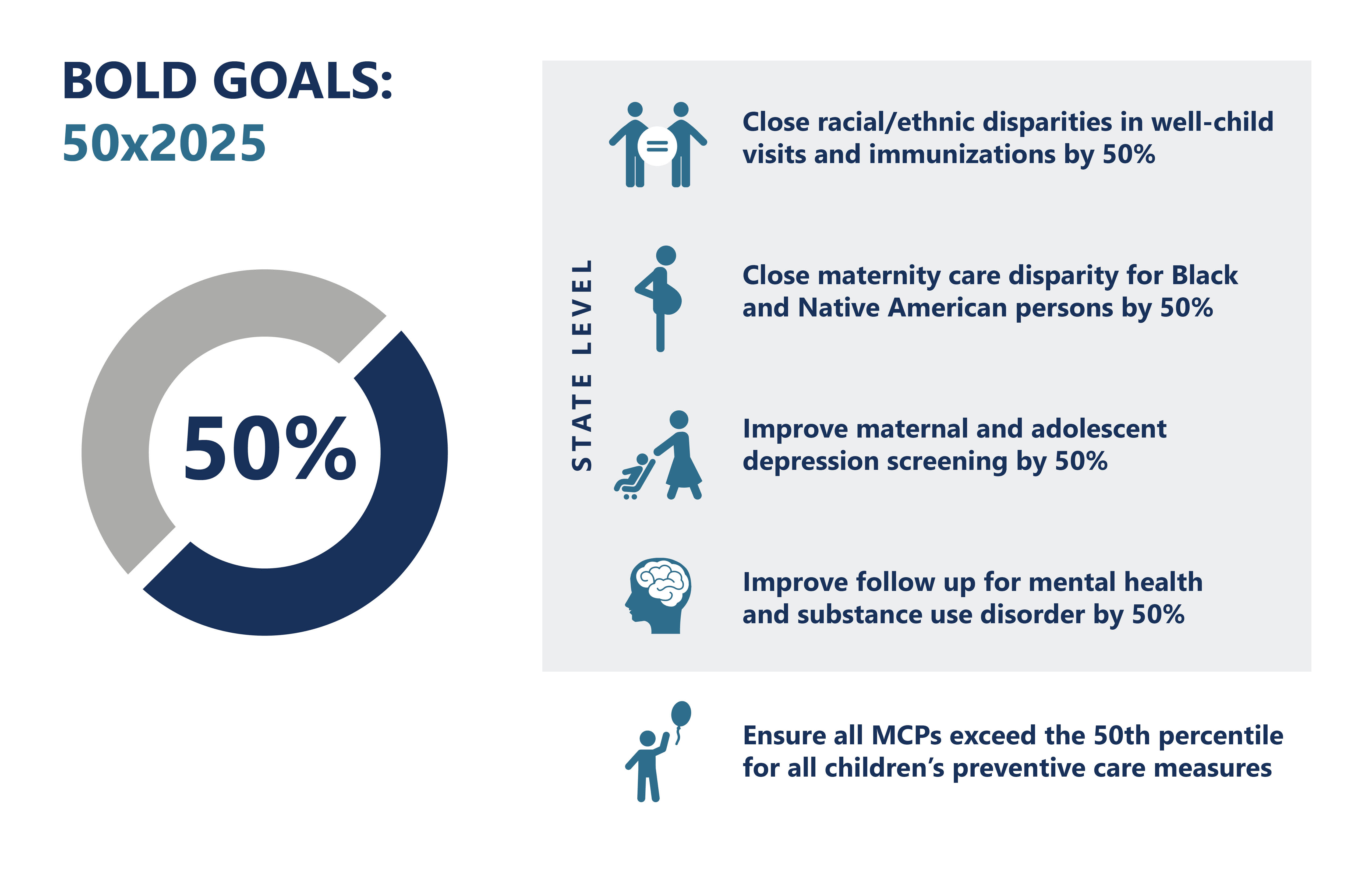
Population Health Management approach grounded in high-quality primary care as well as the 50x2025 Bold Goals Initiative to improve health care outcomes for children's preventive health, maternity care and birth equity, and behavioral health integration.
Centering Member Voices
Central to DHCS' vision for quality and health equity is the belief that Medi-Cal members are at the center of our policy design and programs.
Health Equity Roadmap: The
Health Equity Roadmap outlines DHCS' plan to reduce health disparities by collecting data, identifying care gaps, and creating targeted interventions for high-risk groups. A statewide listening tour gathered member feedback directly from communities experiencing disparities to help shape this roadmap, which aims to build transparency and trust among diverse members.
Member Advisory Committee: In 2023, DHCS launched the
Medi-Cal Member Advisory Committee (MMAC), a dedicated forum for Medi-Cal members to provide direct feedback to DHCS' Director and executive leadership. The committee is composed entirely of Medi-Cal members and family caregivers, ensuring that a diverse range of perspectives is represented.
Improving Transparency and Accountability for Quality
Quality Measurement in Behavioral Health: While DHCS has long tracked quality performance for Medi-Cal managed care plans (MCP), starting in 2022, DHCS also established a
Behavioral Health Accountability Set (BHAS) to measure clinical quality outcomes in county Behavioral Health Plans.
Improved Transparency: Over the last three years, DHCS significantly increased the amount of public reporting on quality and equity outcomes across delivery systems and initiatives to provide improved transparency and empower partners to use data to drive improvements. This includes, but is not limited to:
Sanctions and Accountability: MCPs failing to meet quality standards may face corrective action plans, financial penalties, or even contract termination in severe cases. Sanctions ensure plans prioritize quality care and improve service delivery where necessary. In the last three years, DHCS has strengthened its policy on quality sanctions for both
MCPs and
Behavioral Health Plans (BHP). Additionally, DHCS levied financial sanctions in 2022, 2023, and 2024 on MCPs that failed to meet DHCS' target for quality outcomes (national 50
th percentile).
Supporting Quality Improvement: DHCS partnered with MCPs on several quality improvement efforts to enhance the care of Medi-Cal members, including:
- Participating in the Centers for Medicare & Medicaid Services (CMS) Infant Well-Child Visit Learning Collaborative.
- Creating new regional collaboratives for all MCPs to discuss regional barriers, disparities, and potential community partners.
- Hosting the DHCS Quality & Health Equity Conference in 2023 as a forum for plans to share and network successful strategies in quality and equity improvement.
- Launching two new statewide learning collaboratives in 2024, one focused on improving and scaling children's preventive services and the other focused on behavioral health integration and improved collaboration between MCPs and county behavioral health plans.
Financial Incentives to Drive Quality & Equity
Quality Withhold and Incentive Program: In 2024, DHCS implemented a
Quality Withhold and Incentive (QWI) program. The program incentivizes MCPs to improve performance on quality metrics that align with the DHCS Comprehensive Quality Strategy and Bold Goals by withholding 0.5% of capitated payments, which can be earned back by meeting performance targets for quality, patient satisfaction, and efficiency.
Auto-Assignment Incentive Program: This program rewards higher performing MCPs in certain counties (with more than one MCP) with a greater percentage of new Medi-Cal members (who do not actively choose a MCP). In 2024, DHCS revised this long-standing
Auto-Assignment Program to focus solely on MCP performance on select quality measures aligned with its Comprehensive Quality Strategy and Bold Goals.
Primary Care Spending and Alternative Payment Models: Starting in 2024, all MCPs are required to report to DHCS on what percentage of their spending is going toward primary care and how they are using alternative payment models with providers to reward quality and equity. DHCS worked with key state partners, including Covered California and CalPERS, to
align these contract requirements across public purchasers.
Equity and Practice Transformation Payments: In 2024, DHCS launched the
Equity and Practice Transformation Payment Program, a $140 million investment in primary care practices to advance health equity and reduce disparities by working on upstream care models, improving quality of care, value-based payment models, and practice transformation.
Investing in Communities
MCP Community Reinvestments: Starting in 2024, all MCPs that make a profit are required to reinvest 7.5-15% of that profit in community reinvestment activities that are informed and guided by local community needs.
California Advancing and Innovating Medi-Cal (CalAIM):
CalAIM seeks to improve care for Medi-Cal members through Enhanced Care Management and
Community Supports services, like housing navigation, medically tailored meals, and recovery housing, as alternatives to traditional medical services.
Behavioral Health Services: DHCS has significantly increased investments to expand telehealth, integrate behavioral health with primary care, and support the
Behavioral Health Continuum Infrastructure Program (BHCIP) to build new treatment and community-based facilities.
-
BH-CONNECT and
Behavioral Health Transformation initiatives are enhancing access to care by providing coordinated outreach, navigation, and engagement services to individuals in need of behavioral health support.