BCCTP Applicant Section
BCCTP is here to help! The information on this page will help you understand if you may qualify for benefits, ways to submit an application, and answers to frequently asked questions. If you already have BCCTP benefits, you can go to the BCCTP Member webpage for information.
There are BCCTP Medi-Cal Changes coming in 2026!
Enrollment Freeze
Starting January 1, 2026, some new BCCTP adult applicants will no longer be able to sign up for full scope BCCTP Medi-Cal coverage based on their immigration status. However, eligible applicants may still receive limited scope BCCTP Medi-Cal to cover treatment for breast and cervical cancer.
Medi-Cal Help Resources
Can I get BCCTP benefits?
You may be eligible for the BCCTP program if you:
- Live in California
- Have breast and/or cervical cancer and need treatment
- Your monthly paycheck (gross income) is less than $2,510 before taxes are taken out for a household size of one (1) person.
- Note: The monthly income changes based on the number of people in your household. If you are unsure if your income would make you eligible, but you meet the other criteria, you should apply.
If you are age 65 or older, or have other coverage, you can still get benefits.
Your monthly income is important to see if you can get and keep your BCCTP benefits. The number of people in your family living with you at the time you apply is also very important.
See the income information below.
1
| $31,300 or less
| $2,610 or less
|
2
| $42,300 or less
| $3,526 or less
|
3
| $53,300 or less
| $4,442 or less |
4
| $64,300 or less
| $5,360 or less
|
5
| $75,300 or less
| $6,276 or less
|
6
| $86,300 or less
| $7,192 or less
|
7
| $97,300 or less
| $8,110 or less
|
8
| $108,300 or less | $9,026 or less
|
9
| $119,300 or less
| $9,942 or less
|
10
| $130,300 or less
| $10,860 or less
|
Here is a video that tells you about the different types of income:
What is Income?
For BCCTP, the family size is the total number of persons in the home which includes the applicant, spouse, and their children under 21.
Here are two examples of individuals who can get BCCTP benefits:
Example 1: I live with my spouse and my 21-year-old child. I get $1,000 each month from State Disability Insurance (SDI). My spouse also gets $1,500 each month from Social Security. My 21-year-old child gets $3,500 each month from their job.
In this situation, the only income that matters are mine and my spouse’s. Our 21-year-old child’s income does not matter.
My Income: $1,000
My Spouse's Income + $1,500
My 21-Year-Old Child's Income Does not matter
______________________
Total Income for BCCTP: $2,500
Example 2:
I live with my spouse, my 21-year-old child, and my two young grandchildren. Each month I get $1,800 from my job. My spouse does not work and has no income. My 21-year-old child works and gets $1,500 each month from their job.
In this situation, only my income matters. Our 21-year-old child’s income does not matter.
My Income: $1,800
My Spouse's Income + $ 0
My 21-Year-Old Child's Income Does not matter
________________________
Total Income for BCCTP: $1,800
How to Apply
If you meet the criteria for the program, or think you may, there are three ways to apply for BCCTP.
1. Visit an Every Woman Counts (EWC) Program Provider
Every Woman Counts (EWC) provides free breast and cervical cancer screening and diagnosis services, at places close to you, if you meet certain requirements. To learn more about whether you qualify for breast cancer and cervical cancer screening and diagnostic services, visit the Every Woman Counts Program Webpage.
You can find a local Every Woman Counts Program medical provider by going to the EWC Provider Location Tool. An EWC provider can help you apply for BCCTP.
If you want to speak with someone about Every Woman Counts, you can call the numbers below:
Breast Cancer Screening and Diagnostics
- Call (800) 511-2300
- Help is here 24/7
- We speak English, Spanish, Arabic, Armenian, Cambodian/Khmer, Cantonese, Farsi, Hindi, Hmong, Japanese, Korean, Laotian, Mandarin, Punjabi, Russian, Tagalog, Thai, and Vietnamese
Cervical Cancer Prevention
- Call (800) 511-2300
- Help is here 24/7
2. Family Planning, Access, Care and Treatment (Family PACT) Program
The Family PACT Program provides family planning and reproductive health services at no cost to California’s low-income residents of reproductive age. The main goal of the Family PACT Program is to make sure that low-income women and men have access to health information, counseling, and family planning services to maintain their best reproductive health. These providers can help you apply for the BCCTP program. To find a Family PACT provider close to you, go to the Family PACT Provider Locator.
3. Apply at your County Social Services Office
A worker at your county office is there to help! You can find a local office by going to the County Offices Webpage.
If your doctor told you that you have a breast and/or cervical cancer diagnosis, tell one of the county workers so that they can send your information to BCCTP. A BCCTP Eligibility Specialist will reach out to you directly to start an application.
The county worker will also take your information to see if you can get free Medi-Cal benefits, or if you can get Medi-Cal with a share-of-cost. Your county worker can provide you additional information about share-of-cost Medi-Cal.
BCCTP is here to support you during the application process. Contact us if you need help by calling 1-800-824-0088 or emailing BCCTP@dhcs.ca.gov. Leave us your name and a good phone number where we can reach you.
If you need someone to help you or obtain information on your behalf, complete the Authorized Representative forms below.
- MC 382 - Appointment of Authorized Representative
- MC 383 - Authorized Representative Standard Agreement for Organizations
Frequently Asked Questions (FAQs)
What benefits do I receive if I apply for BCCTP?
Your BCCTP benefit is Medi-Cal coverage. Talk to someone who can explain your benefits to you. Member Benefits/Provider Support can tell you the kinds of health care services you can use, based on your specific benefits. Just call (800) 541-5555.
What do I do if I need help paying my health insurance premium?
Do you have Medicare or other health insurance? If so, you may still be eligible for BCCTP. BCCTP can even reimburse your premiums for your other health insurance. You need to have out-of-pocket expenses more than $750 each year on that other health coverage.
How long do BCCTP benefits last?
You can access needed care as long as you need cancer treatment and meet other criteria. You must return an annual renewal packet, which will be sent to you every 12 months by mail. You must return it by the due date on the packet, or you may lose your BCCTP benefits.
What happens after I apply for BCCTP?
An eligibility specialist will assess your application to enroll you if you are eligible for the program. We may need to ask you for more information to understand your situation better. You will receive a notice to inform you if you are approved or denied. You may receive a separate notice from your county social services office regarding your Medi-Cal application.
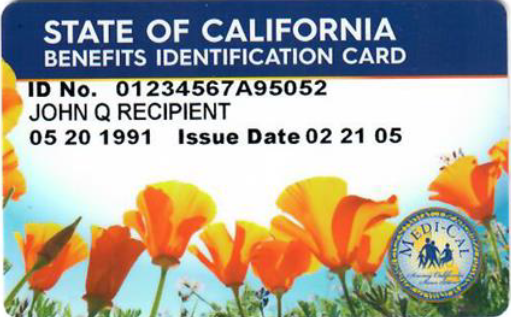
If you qualify for BCCTP or Medi-Cal, you will get a Medi-Cal card (also called a Benefits Identification Card or “BIC”) in the mail. You should show your Medi-Cal card at every medical appointment and at the pharmacy when you pick up medication. Your providers use it to view your BCCTP benefits and see if your services are covered.
The Medi-Cal card looks like this:
What is Retroactive Medi-Cal?
Retroactive Medi-Cal benefits may cover the cost of medical services and treatment you received during the 90 days right before you applied for BCCTP benefits, if you are eligible. BCCTP will send you a form to complete, which you must send back for Medi-Cal to pay the bill or receive reimbursement.
When you apply for Medi-Cal at the county, tell your worker you need retroactive Medi-Cal.
How do I contact BCCTP?
Department of Health Care Services
Medi-Cal Eligibility Division
Breast and Cervical Cancer Treatment Program
P.O. Box 997417, MS 4611
Sacramento, CA 95899-7417
What If I am not eligible for BCCTP?
If you do not qualify for BCCTP but need health insurance coverage, you may qualify for low-cost coverage from
Covered California. Apply online or call them at (800) 300-1506 (TTY: (888) 889-4500).
Other Insurance and Medical Resources:
